After a family member broke a hip recently, I decided I’d better look into treatments for osteoporosis. There is strong observational evidence that reduced bone density increases the risk of broken bones. In turn, many large drug trials give experimental evidence that increasing bone mineral density reduces the risk of fractures. Drugs from the 90s are effective and safe and now available as cheap generics. Newer drugs are more powerful, though much more expensive.
Diagnosis and Fracture Risk
Bone mineral density (BMD) is best measured by dual energy x-ray absorptiometry, or DEXA scans, which are widely available outside of medical settings because they’re also used to measure body fat percentage. BMD results are reported three ways. The raw result is in mg/cm^2. A z-score reports a patient’s BMD in standard deviations from the mean of people their age, sex, and race. A t-score compares BMD to young adults at their maximum BMD instead of to people of the same age as the patient. The reference points for t-scores and z-scores have shifted a bit over the years, but, in the US, come from the NHANES program.
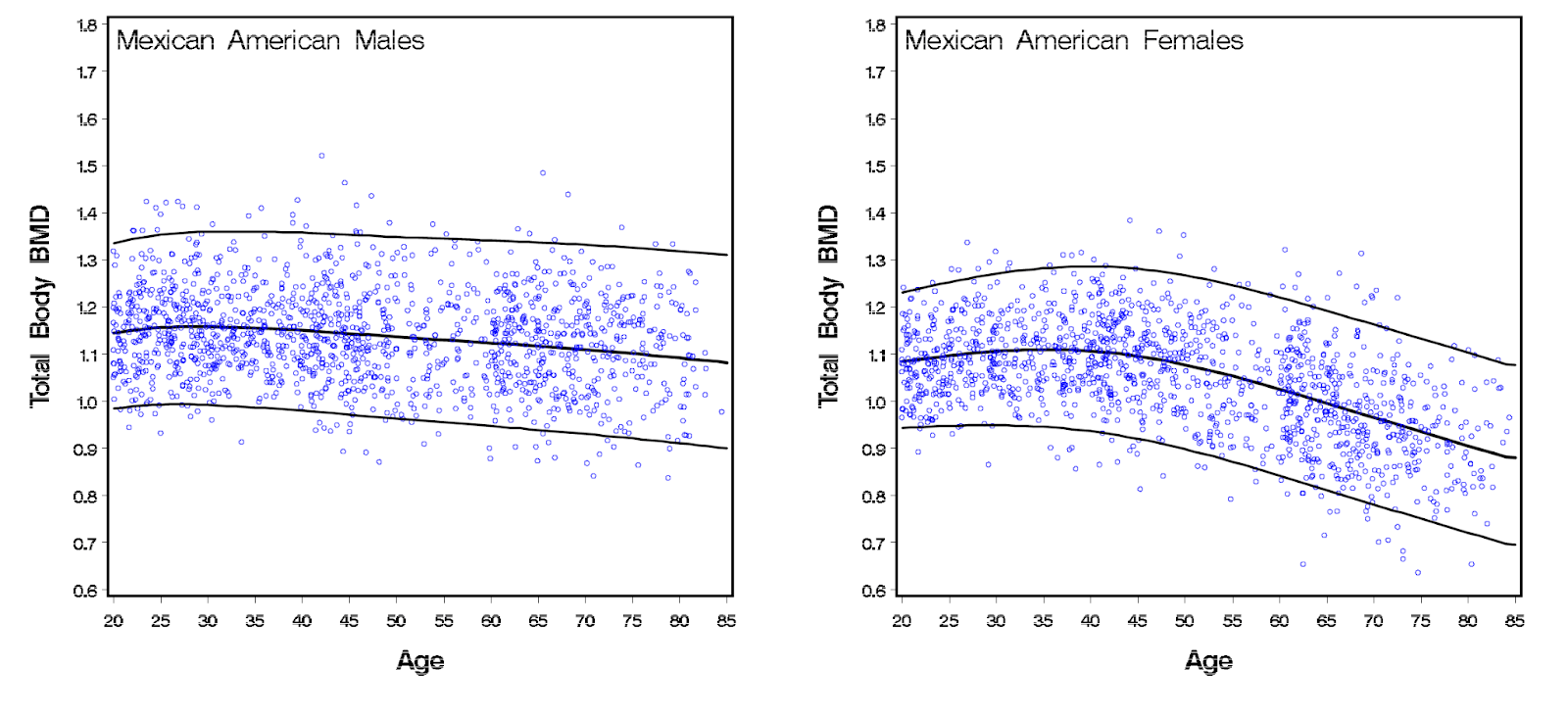
Osteoporosis is defined as a t-score of -2.5 or below. Diagnosis lasts for a lifetime. Even if treatment raises the t-score above -2.5, patients still need to have their BMD monitored and treated. Below are plots of BMD by age from NHANES in 2009 (more recent results, which might use different categories for race and ethnicity, are stuck behind a paywall). BMD declines most quickly for women over 50, but declines for men too.


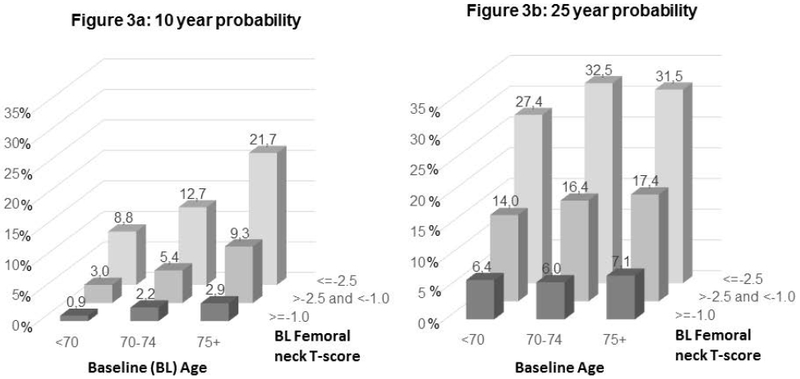
There is strong observational evidence linking lower BMD to fracture risk. The Study of Osteoporotic Fractures, a 25-year observational study of 8,000 women, demonstrates that age and baseline BMD – measured at the point where the femur connects to the hip – both contribute to the risk of a broken hip (plot below). The effect of BMD is much stronger than the effect of age, though. The Fracture Risk Assessment Tool is a convenient calculator for estimating the 10-year risk of breaking a hip or other major bone for people 40-90 years old. You can use it without knowing your BMD, though including BMD makes it more accurate.
Treatment
Phase 3 drug trials for osteoporosis are required to show not just an increase in BMD, but a reduction in fractures. The studies have two common ways of measuring fractures. One is to focus on what they call clinical fractures, meaning the patient knows they broke a bone. A second measure is vertebral fractures, or spine fractures, often measured as “radiographic” or “morphometric”, which the patient may not know they have. They’re often defined as a 4 mm reduction in the distance between vertebrae. Most trials study patients with both osteoporosis and pre-existing breaks, which puts them at the highest risk for new breaks.
As an aside about the importance of spine fractures, at least one drug trial measured whether people got shorter, but even in the control group there was no change in height, as funny as it would have been. The same trial found their drug caused a 71% reduction in reports of back pain. So these fractures do matter, even if they don’t present in the same abrupt and extreme way as a broken hip or wrist. Most studies didn’t track height or back pain, though.
A 2018 meta-analysis of 38 trials for 19 drugs found a strong link between how much the drugs increased BMD and how much they decreased both spine and hip fractures. They did not find a link to the broader category of nonvertebral fractures, which in addition to hips includes wrists, arms, and legs. These other kinds of breaks may more commonly be related to trauma than bone density.
The oldest and largest category of drugs for osteoporosis is bisphosphonates. They can be given orally or intravenously at frequencies from daily to yearly. These drugs are still the first-line treatment. The oral versions are available as low-cost generics. Their side effects are well understood. The most commonly reported side effects are indigestion, abdominal pain, nausea, and heartburn, though randomized trials find nearly equivalent side effects on placebo.
There are two serious but rare side effects of bisphosphonates. First is osteonecrosis of the jaw (ONJ), in which parts of the jawbone become exposed through the gums. However, a consensus statement in Osteoporosis International says, “For patients taking oral bisphosphonates to manage osteoporosis, the incidence of ONJ is estimated to be between 1/10,000 and 1/100,000 and is only slightly higher than the ONJ incidence in the general population.” The second serious side effect is atypical femur fracture (AFF). The same consensus statement finds that, “For patients taking bisphosphonates for osteoporosis, the absolute risk of AFF is low: ranging between 3.2 and 50 cases/100,000 person-years, an estimate that appears to double with prolonged duration of bisphosphonate use (> 3 years, median duration 7 years), and decline rapidly with discontinuation.” These side effects are why it’s standard practice to take a “holiday” of up to 5 years after receiving 5 years of oral treatment or 3 years of intravenous treatment.
Here’s a quick roundup the main bisphosphonates
- Alendronate (Fosamax)
- The Fracture Intervention Trial in women with low BMD and pre-existing spin fractures – treatment over 3 years reduced new spine fractures by 47% and clinical fractures by 28%.
- The Fracture Interventions Trial in women with low BMD but without pre-existing spine fractures – treatment over 4 years reduced vertebral fractures by 44% and clinical fractures by 14%, which missed statistical significance. In women with osteoporosis (some women in the trial had the milder osteopenia) the reduction in clinical fractures was 36%, which did hit statistical significance.
- Risedronate (Actonel)
- VERT USA – over 3 years, new spine fractures reduced by 41% in women with pre-existing spine fractures.
- VERT Europe – over 3 years, new spine fractures reduced by 49% in women with pre-existing spine fractures.
- Ibandronate (Boniva)
- RCT – daily and quarterly oral dosing versus placebo reduced new spine fractures by 62% and 50% and clinical spine fractures by 49% and 48%.
- Zoledronic acid (Reclast)
- RCT – Annual intravenous infusion reduced new radiographic spine fractures 70% and hip fractures 41%. Statistically significant side effects included a 0.8% absolute increase in atrial fibrillation. The (company sponsored) trial authors suggest this was a fluke. Nearly all cases happened more than 30 days after infusion, when the drug was no longer circulating. They claim there’s no biological mechanism to connect the drug to afib. There were also side effects around the day of infusion. After the first infusion, 1/3rd of patients had flu-like symptoms, 7% did after the second injection, and 3% did after the third.
BMD is controlled by the constant turnover of bone – old bone tissue is broken down and new tissue is created. Bisphosphonates slow down that breakdown process. Denosumab (Prolia/Xgeva) is a monoclonal antibody that works similarly, slowing bone breakdown. The initial drug trial found that subcutaneous injection every 6 months reduced the risk of new radiographic spine fractures by 68% and hip fractures by 40% compared to placebo. That effect sounds larger than for bisphosphonates, but a meta-analysis of head-to-head trials shows it’s not any more effective than bisphosphonates.
Another class of new drugs, anabolic agents, stimulate new bone formation. Two are Parathyroid Hormone Related Protein (PTHrP) analogs.
- Teriparatide (aka parathyroid hormone (1-34), brand name Forteo)
- RCT vs placebo – Daily subcutaneous injection reduced new radiographic spine fractures by 65% at low dose and 69% at high dose and other fractures by 53%.
- RCT vs risedronate – Women on teriparatide had 56% fewer new spine fractures and 52% fewer clinical fractures.
- RCT vs alendronate – Teriparatide caused a 70% reduction in nonvertebral breaks. This was the trial that found no change in height but a large decrease in back pain. It also found leg cramps increased from 0 to 8.2% on treatment, kind of like growing pains?
- Abaloparatide (Tymlos)
- RCT – Daily subcutaneous injection reduced new radiographic spine fractures by 86% and other fractures by 43%. Effects were larger than (open-label) teriparatide with lower rates of hypercalcemia. Nonvertebral fractures were 30% lower than in teriparatide, but that comparison was open-label and underpowered.
Lastly, romosozumab (Evenity) is another new medication used to build bone. It’s a monoclonal antibody that works by blocking the effects of sclerostin, a protein that inhibits bone formation.
- RCT – Monthly subcutaneous injection versus daily oral alendronate. Treatment only lasted 12 months, after which all patients took open-label alendronate, but the primary endpoint was measured at 24 months. The trial found a 48% reduction in new spine fractures and a 38% reduction in hip fractures. Serious CVD events during year 1 increased from 1.9% to 2.5%.
Besides their more potent effects, the other benefit of these new anabolic agents is that they have a faster impact than bisphosphonates. The Endocrine Society Clinical Practice Guideline recommends that the highest risk patients – those recovering from a hip fracture or with multiple vertebral fractures, and who also have osteoporosis – get treated with anabolic agents first, followed by bisphosphonates. For some reason, BMD regresses faster after patients go off anabolic agents than bisphosphonates, so patients should not go directly from anabolic agents to a drug holiday.
Osteoporosis in men
The clinical guidelines for osteoporosis say that “men aged ≥ 50 years with history of adult-age fracture” should receive BMD testing. Furthermore, “to detect subclinical vertebral fractures, perform vertebral fracture imaging” in “men aged ≥ 50 years with…Fracture(s) during adulthood (any cause).” And finally, “consider initiating pharmacologic treatment in postmenopausal women and men ≥ 50 years of age who have…Fracture of the hip or vertebra regardless of BMD.”
Although all of the trials above were conducted in postmenopausal women, “All FDA-approved medications to treat osteoporosis in men have been demonstrated in RCTs to increase BMD.” A meta-analysis of bisphosphonate trials in men found a 63% reduction in spine fractures and a 40% reduction in other fractures.

